
So, just how much do unspecified HCCs really cost your organization?
To better understand what unspecified HCC coding might be costing you, lets first break down Risk Adjustment Factor. Risk Adjustment Factor score measures how costly a patient is predicted to be for the current year. Within Value-based care models, patients in the same practice could have dramatically different payment rates. A multitude of factors determine the amount of risk and work involved to maintain the health of a patient. A patients RAF score is heavily weighted on HCC’s.
A lot of the work for HCC falls to the coders, to ensure that each patient’s medical record is coded accurately and that there is the supporting documentation regarding the status of the condition. The goal has always been to code to the highest level of specificity, and it’s essential to the success of the Risk Adjustment program. While most doctors document reasonably well for medical care, many are unaware of the details needed for accurate code selection for billing, reimbursement, and quality measure purposes. Since most of the burden in documenting for RAF scores is up to the provider, implementing programs within your practice or health care organization such as a Clinical Documentation Improvement (CDI) Program can help bridge that gap between provider and HCC coding.
Here’s a simple example
A single patient example helps to convey how critical it is to ensure accurate coding for patients. A female with a weight of 240 lbs. resulting in a BMI of 44 is diagnosed with obesity using ICD-10 code E66.9. This unspecific obesity diagnosis code for this patient has no HCC relevance, which means the patient’s RAF score remains at .000 and payers are unaware of the risk this patient’s weight has on her health and potential cost of care. The more precise and accurate coding of morbid obesity using the E66.01 Dx code would result in a RAF score of .368 for that patient. Figure 1 demonstrates the financial result of more accurate coding for this (normally $800 per member per month costing) patient based only on the addition of a more precise diagnosis coding.
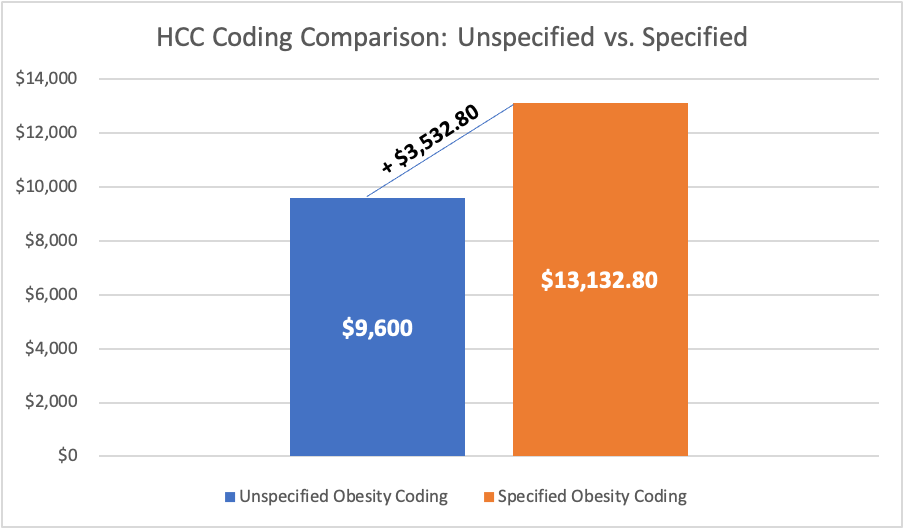
This is why accuracy is so important
The financial impact of optimizing HCC coding is significant as it directly impacts the reimbursement received by a healthcare organization. Mid-size organizations have been known to lose millions of dollars because of low HCC confirmation rates. Correctly coding HCCs predicts the future financial resources for patients and ensures appropriate reimbursement for physicians. For physician leaders, the ability to document with greater precision can dramatically impact revenue.
Some of the challenges
Award winning resources
ReportingMD provides award-winning resources, and the insight necessary to gain a 360 view of your patient population.
From RPM and risk stratification, to provider performance benchmarking and advanced analytics, the ReportingMD team and technology work together to provide an end-to-end solution for Value-Based program management.
We help identify and aggregate the necessary information, merging data from multiple systems into our single platform. Our platform is secure, easy to use and compatible with any EMR / PM technology.
We help identify and manage costly care-gaps to help you provide the best care possible, and thrive in a value-driven environment. With the power to manage multiple TINs and drill-down to the individual patient, we help you gain actionable insights from a seemingly impossible array of information.
See why 1,000’s of providers rely on our services to manage care, risk and performance. Schedule a brief, no-obligation demo today.