Healthcare quality pay-for-performance (P4P) reporting isn’t easy. This truth has existed since the era of the Physician Quality Reporting System (PQRS), Meaningful Use and continues today in the ever-changing Merit-Based Incentive Payment System (MIPS) track, under the 2015 MACRA legislation’s Quality Payment Program (QPP). If programmatic conditions remained static over time, clinicians and practices could eventually find organizational processes to manage interleaving decision points and activities that would ultimately construct a sound (yet complacent) quality management framework. The problem is that static healthcare quality equals static patient care and population health. Therefore, the MIPS program must be variable and able to shift in order to transform the state of our healthcare cost and quality infrastructure. Each variable presents both technical and financial challenges to practice and clinician stakeholders; the results of which have massive impacts on staffing, administration, and clinician time/resources. Finding the best MIPS reporting pathway and solution should be the priority in your annual MIPS reporting strategy planning.
MIPS is composed of four categories, each focused on different elements of the patient care continuum.
- Quality Category: clinicians/practices choose from a set of clinical measures to report on for a full calendar year
- Cost Category: CMS collects cost data for Medicare Spending Per Beneficiary inpatient hospital stays, Total Per Capita Costs, and several episodes-based cost measures calculated only for items and services related to the episode of care for a clinical condition or procedure
- Improvement Activities (IA) Category: clinicians/practices choose from a set of activities identified as improving clinical practice or care delivery, to report on for a 90-day window during a calendar year
- Promoting Interoperability (PI) Category: (eligible) clinicians/practices report for a 90-day period on a set of measures focused on the use of Electronic Health Record (EHR) systems aimed at interoperability and improving patient access to their health information
The complexity of MIPS is not only built into the range of options that make up each of the four categories but also in the range of eligibility/special-status particulars, scoring methodologies, and performance thresholds.
Clinicians and practices must make critical, and often overwhelming, decisions about how they will manage the plethora of reporting factors and requirements under the MIPS program. A deeper dive into the MIPS quality category details this struggle with the wide range of options for how and what should be reported versus how and what must be reported.
Under quality, MIPS ECs and practices must choose what submission method(s) they will employ. Options include: qualified registries/QCDRs, EHR, claims (small practices only), and CMS web-interface. 2019 is the first year when multiple submission methods can be used to fulfill the category reporting requirements, making decisions about submission method(s) even more complicated. With the different options for how to report and the cost, both from the financial and resource availability perspective, clinicians and practices need to consider their individual reporting needs based on the following criteria:
- MIPS Program Strategy and Goals
- Guidance
- Overall scoring including bonus points
- Practice Make-up and Measure Selection
- measure selection
- outcome/HP measure selection
- Measure value ratings
- Practice Systems / Data Sources
- Discrete data fields
- Multiple EHRs require data aggregation
- MIPS Program Strategy and Goals
As stated in the introduction, pay-for-performance reporting isn’t easy. Clinicians and practices typically don’t have time or staffing available to devote to learning all the essentials to consider when developing a sound MIPS strategy. Many EHRs, for example, do not focus on being MIPS program experts and, therefore, fail to offer clinicians and practices many of the required elements to succeed at MIPS.
EHRs, including the applications and the vendor support, are focused on providing systems and services focused on clinical documentation. That is and should be their primary focus. Without providing the necessary program guidance in combination with typically only offering a short list of electronic quality measures, EHRs reporting puts clinicians and practices at a disadvantage when developing a MIPS strategy that maximizes performance to achieve the highest possible upward payment adjustment.
The claims and CMS web-interface submission methods fall off any recommended submission method list because they both rely on CMS to calculate what is reported on based on the claims submitted. Programmatic support for these two methods requires either a dedicated team experienced and knowledgeable in how and what is reported or a lengthy bureaucratic endeavor to get programmatic answers from a government help desk system. The program is far too complex to reply on either the claims or web-interface submission methods.
There is a short list of qualified registries that provide the programmatic guidance, reporting functionality, and expert performance advice needed for a sound MIPS strategy. These qualified registries present detailed scoring information across all reportable MIPS categories including quality, Improvement Activities (IA), and Promoting Interoperability including additional bonus points like small, complex, and year-over-year improvement. Additionally, since not all MIPS ECs and practices are required to report on all MIPS categories, resulting in varying category weights, qualified registries can express the MIPS value story in a way that is unique to these organizations.
Planning for and executing a perfect MIPS strategy requires the ability to understand the complete MIPS scoring story. Without an experienced and knowledgeable support system, a smart MIPS strategy is virtually impossible to achieve.
Practice Make-up / Measure Selection
Practices come in all shapes, sizes, and specialties and each individual practice needs a large selection of quality measures to draw from to reach maximum scoring potential and the highest payment adjustments. Limited options for measure selection create a scoring hindrance that can result in tens or even hundreds of thousands of dollars in Medicare incentive revenue.
In 2019, many EHRs offer just 50 quality measures to choose from, down from both 2017 and 2018. EHR measures, that can score above 3 points, make up only 17% of all measures that can score above 3 points across all submission methods. Moreover, when practices and providers find that their performance is lower than expected, it is critical that they choose outcome and high priority measures beyond the minimum requirement to close the performance-based scoring gap with bonus points. EHR measures have the fewest of these gap-closing outcome and high priority measures
Qualified registries offer over 230 different measures to report on. Registry measures, that can score more than 3 points per measure, make up 62% of all measures that can score above 3 points across all submission methods. 71% of all registry measures are categorized as high priority and/or outcome measures, which offer clinicians and practices bonus points for reporting beyond the minimum criteria. 43% of all registry measures offer both the ability to score above the 3 point minimum and bonus points for being high priority and/or outcome.
Understanding the potential value of a measure can be difficult. When considering which measures to report on, it is helpful to assess measure value based on a rating system from 3 to 20 points, with 20 being the maximum possible value of a measure. This scoring system can also be used to compare the trajectory of measure value by submission method over time. Figure 1 below displays the cumulative measure values forth EHR measures and for registry measures from 2018 to 2019.
Because EHR measures make up such a small number of the full measure spectrum, the cumulative measure value is significantly less for EHR measures than it is for registry measures. As displayed in figure 1 below, the blue line pushing up in the chart is the cumulative value of all registry measures in 2019, which is in stark contrast to the orange line representing the cumulative measure value for EHR measures in 2019.
Figure 1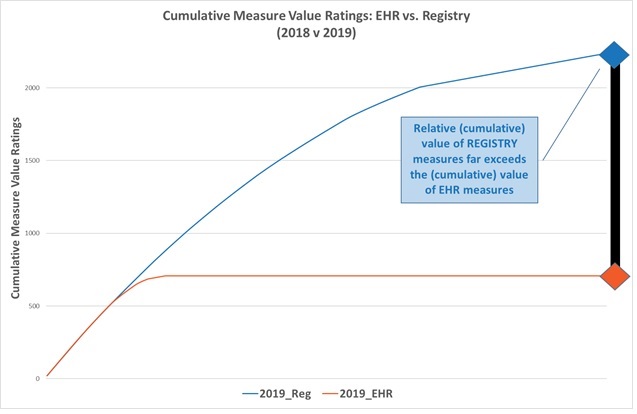
Additionally, EHR measures have a value track that inherently decreases over time. The reason is that many clinicians and practices are reporting on fewer measures and are focused on improving on a shorter list of clinical actions and processes. This fact forces EHR measure values to be topped-out sooner, which drives down their measure value at a faster pace than that of registry measures. This fact is demonstrated in figure 2, which shows the measure value trajectory of registry measures from 2018 to 2019 versus the trajectory for EHR measures from 2018 to 2019. The slope of the registry measure value line is increasing year over year while the slope of the EHR measure value line is decreasing year over year.
Figure 2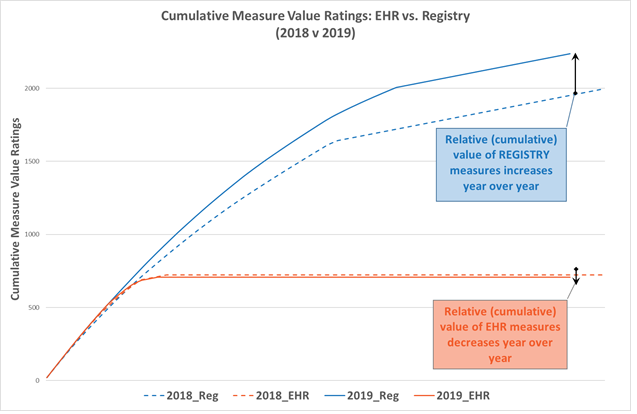
Practice Systems / Data Sources
Reaching beyond programmatic support and intrinsic measure value, it is also critical for clinicians and practices to understand what data they have available and how to access that data for accurate and successful reporting. Practices come in several shades of health IT (HIT) systems being utilized. Some use a single HIT platform for all billing and clinical data management while others utilize system(s) specifically designed to manage billing data versus those that specifically manage clinical data. There are also many practices that utilize more than two HIT systems. Regardless of the variety of IT systems utilized, practices need to understand their clinical processes, how those processes are documented electronically, and how to access that data for reporting.
Using EHRs for reporting requires pinpoint accuracy in the use of discrete data fields, as those data fields are what the EHRs use to aggregate the results for measure reporting. Experience demonstrates that no two physicians utilize an EHR in the same way, let alone two different practices. If the specific language/documentation is not used in exactly the right data field within an EHR, the provider/practice may be missing out on performance points they deserve based on clinical care but don’t receive based on EHR utilization. This is one of the reasons that EHR reporting can be difficult and cause practices to suffer from scoring disadvantages.
Registries, especially those with ONC certification (to be able to report on the EHR measures in addition to the registry measures), offer the largest measure selection and the ability to pull data from discrete data fields as well as from alternative data sources and locations like a notes field, for example. Clinicians and practices can therefore maximize their scoring because they are getting credit for all the clinical activity they do and not just what is documented perfectly in exactly the right location.
Discrete data fields are not the only system challenge that clinicians and practices face. Because many practices use multiple HIT systems (e.g. Practice Management (PM) systems, EHRs, and in some cases more than one EHR), they must be able to aggregate data from disparate systems, often with variable patient identification, in order to report accurately for MIPS measures.
This is another subject where EHRs faulter. Practices using multiple HIT systems must report accurately on the complete population even if that population is covered across multiple systems. Practices must be able to pull together data from multiple different HIT systems, often with different patient identifiers. Since different systems don’t “speak the same language” or have data connectors to aggregate data correctly, accurate EHR reporting is rarely achieved.
Some qualified registries, especially those with ONC certification (to be able to report on the EHR measures in addition to the registry measures), are experts in aggregating data across multiple systems including those using individual patient identifiers. This unique expertise is necessary in order to collect all required reporting and performance data needed to accurately report under the MIPS program. Practices that don’t submit complete data from all HIT systems are at a significant risk of losing out on performance data and even the possibility of CMS audit based on incomplete reporting.
CMS estimated that clinicians and practices who report through registries/QCDRs was expected to increase by over 27% from 2018 to 2019[i]. This is good news for some of those practices since the value story of the MIPS program is in utilizing an expert registry vendor that can maximize the practice’s MIPS payment adjustment earning potential. Not all qualified registries offer all necessary elements to reach optimal MIPS reporting so it is critical that practices do their due diligence to find the idea registry, which should include/offer:
- Programmatic experts for optimal guidance and support
- Measure experts for precise measure aggregation
- Data experts for accurate and comprehensive data collection
- Health IT/data system experts to connect all relevant data across disparate Health IT systems
- Submission experts to review submission results and opportunities for improvement
Qualified registries that encompass those elements for successful reporting will have the primary objective and the most skills and expertise to create the maximum earning potential for clinicians and practices under P4P programs. Maximizing the relationship by including the ideal registry vendor in as a stakeholder or quality partner in the pursuit of P4P program reporting is the best chance for a practice to achieve the best possible MIPS strategy. A strategy that incorporates the maximum reporting options along with the ability to pull together all necessary data from all relevant sources to report accurately and achieve the highest possible upward adjustment.
About the Author:
Molly Minehan is ReportingMD’s Director of Client Services and Innovation
[i] Center for Medicare and Medicaid Services, 2018. Medicare Program; Revisions to Payment Policies under the Physician Fee Schedule and Other Revisions to Part B for CY 2019; Medicare Shared Savings Program requirements;
Quality Payment Program; Medicaid Promoting Interoperability Program; Quality Payment Program–Extreme and Uncontrollable Circumstance Policy for the 2019 MIPS Payment Year; Provisions from the Medicare Shared Savings Program–Accountable Care Organizations–Pathways to Success; and Expanding the Use of Telehealth Services for the Treatment of Opioid Use Disorder under the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act. Department of Health and Human Services, 83 FR 59452. https://federalregister.gov/d/2018-24170

